Changing the culture of patient safety
By Jan Jarvis
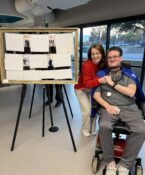
Scott Carlton, 7, with his private duty nurse, Olubunmi Ogundoju.
Patient Safety SummitThe Institute’s annual Patient Safety Summit is scheduled for Oct. 27-28 in Fort Worth. The conference, “Drive the Difference: Leading Innovation in Patient Safety” will focus on delivering safer care in ambulatory settings. The InstituteThe Institute for Patient Safety focuses on research, quality improvement projects and mentoring of students and faculty. Organizations that participate in academic research, higher education or the direct delivery of care will be considered for full membership. Institute FellowsThe inaugural roster of Institute Fellows includes scientists and physicians from UNTHSC, TCU, JPS, Cook Children’s and University of Texas at Arlington. Fellows will work with the university’s faculty to ensure patient safety remains a key component in the curriculums of UNTHSC’s existing graduate programs and in the new MD school being created with TCU. Finding what worksThe Institute will fund small-scale testing of innovative new patient safety concepts through four annual seed grants worth up to $25,000 apiece. It also will award larger project grants, worth up to $100,000 each, for studies that can have an immediate impact on health care. |
Jeff Carlton and his wife were leaving the hospital, two days after learning that their infant son had a rare brain disorder called lissencephaly – and a life expectancy of just two years.
Reviewing the discharge paperwork, the distraught parents from Arlington caught a critical mistake: a misplaced decimal point in the dosage prescribed for a drug to control their son’s seizures.
“I don’t know what 10 times the dosage would do to a 7-week-old kid, but a mistake like that was tough for two emotionally devastated parents to catch,” said Carlton, Director of Media Relations at UNTHSC. “I should not have to do that sort of math on the worst day of my life.”
Though the error was caught in time and caused no harm, it illustrates how a simple mistake can often have huge consequences. Despite protocols to protect patients – from smart pumps to color-coded gowns – an estimated 250,000 Americans die annually due to medical errors, making such mistakes the third most common cause of death in the U.S., according to researchers from Johns Hopkins University.
The financial impact is staggering, too. Medical errors lead to an estimated $50 billion in added U.S. health care costs, and up to $1 trillion in lost human potential and contributions.
Key health care organizations in Fort Worth are pushing for change, starting with the new Institute for Patient Safety at UNT Health Science Center. Founding partners include Cook Children’s Medical Center, JPS Health Network and Texas Christian University.
While the institute takes a broad view of patient safety, it will focus on three areas where it can make a difference: ambulatory care settings, geriatric care and precision medication.
This week, the Institute is hosting its second annual Patient Safety Summit, which will focus on innovative approaches to coordinating and delivering safe, high-quality care in ambulatory settings. Featured speakers include:
- Zubin Damania, MD, Medical Director, Downtown Project Las Vegas
- Andrew Kolodny, MD, Chief Medical Officer, Phoenix House Foundation
- Elizabeth Phillips, MD, Director of Personalized Immunology, Vanderbilt University Medical Center
- Hardeep Singh, MD, MPH, Chief of Health Policy, Baylor College of Medicine
“For 30 years the health care industry has tried to improve patient safety, but in all that time we’ve hardly moved the needle,” said Michael Hicks, MD, Executive Vice President for Clinical Affairs at UNT Health Science Center. “Reducing medical mistakes calls for more than protocols; it calls for cultural change and a new way of doing the business of health care.
“We simply have to expect better.”
Changing the culture
Improving patient safety starts with a big dose of reality.
The new MD school being developed in collaboration with TCU is one example of culture change, Dr. Hicks said. Patient safety won’t be taught as a single subject but will be integrated into the entire curriculum.
“The fact is, mistakes are going to occur,” Dr. Hicks said. “We have to design a system that accounts for human errors. We have made physicians God-like. No one wants to question them, but we should make everyone feel empowered to do exactly do that.”
Senator Jane Nelson, who helped secure $4 million in funding from the Texas Legislature, said the institute will collaborate with other health care and education partners in Texas to improve quality and reduce preventable harm.
“The goal is that the institute will impact the lives of every patient in Texas by creating a universal culture of safety throughout our state,” she said.
The first step is being able to talk about errors without fear, said Dr. Frank Rosinia, Executive Vice President and Chief Quality Officer for JPS.
“We need to have what’s called psychological safety,” he said. “If someone acknowledges a mistake that could harm patients, they should be lauded for it.”
The call for a change in culture starts at the top and reaches everyone, said Joann Sanders, MD, Chief Quality Officer at Cook Children’s, where a hospital-wide safety call takes place every morning at 9 o’clock.
“It takes 15 minutes to get a feel for how the hospital is doing,” she said. “If equipment is down in one department, we know it.”
The bottom line is everyone has to be committed, said Lorrainea Williams, PharmD, Patient and Medical Safety Officer for Cook Children’s.
“There has to be that constant, relentless, drumbeat that everyone shares,” she said.
Nancy and Carl Bluemel
Safeguards that follow the patient
For the Bluemel family, medication management and continuity of care have become important issues after problematic patient experiences for both Carl, 48, and his 76-year-old mother, Nancy.
Carl, who enjoys playing rec-league hockey, recently had inpatient hip surgery. He says he was assured he would receive follow-up care at home from a nurse and physical therapist. But no one ever showed up.
“Someone had put in the order, then they went on vacation and it never got processed,” said Bluemel, Digital Design Director at UNTHSC. “Now I was 46 and not the typical hip replacement patient. But imagine what could have happened if I was 76.”
Meanwhile, after breaking her arm, Nancy Bluemel, 76, was prescribed hydrocodone. But once at home, she became confused and had trouble walking.
Her family worried that she had hit her head or suffered a stroke. Twice they sought medical care. On their third attempt, an ER nurse said she’d seen other elderly patients with similar reactions to the painkiller. When the family moved her to a rehab facility, they asked that she be switched to another medication. But that never happened.
“She was a complete zombie,” said Carl Bluemel. “Even when we pointed it out, the mistake kept happening.”
Older adults are twice as likely as others to come to emergency departments for adverse drug events and nearly seven times more likely to be hospitalized after an emergency visit, according to the Centers for Disease Control and Prevention.
Much has been done to reduce mistakes, from bedside medication verification systems to cautions embedded into electronic health records. But the safeguards don’t always follow patients after they leave hospitals – even though most Americans receive most of their care in outpatient and ambulatory settings.
What is needed is a strong partnership between health care providers, Dr. Rosinia said.
“We need to do a better job of delivering care across the continuum,” he said. “Even in the hospital, we’ve had cases where patients go from one unit to another and their meds don’t follow them.”
Educating caregivers and families

In the age of social media, consumers are quick to speak up when service is poor. It should be no different with health care.
“Nobody has more of a vested interest in safety than patients and their families.” Dr. Hicks said.
As the population ages, expect to see consumer groups such as AARP driving change, said Susan Mace Weeks, Dean and Professor of the Harris College of Nursing & Health Sciences at TCU.
“Their advocacy will improve care of patients and ultimately enhance the health and well-being in the greater community,” she said.
Hospitals also must educate patients in understandable language about how they can protect themselves. Around 40 percent of patients’ caregivers fail health literacy screenings, which has led Cook Children’s to work closer with families, Dr. Sanders said.
“We want them to feel confident that when they get home they will know what to do. If not, they should call us,” Dr. Sanders said. “We don’t want to see them back in the ER when it was something we could have fixed over the phone.”
Still, the stress of hospitalization can rattle even the most medically astute caregiver.
“We were within hours of giving our son a massive and inappropriate dosage of medication,” said Carlton of the close call with his son Scotty, who is now 7. “We were really lucky we caught it.”






Social media