The transforming power of medical education
By Jeff Carlton
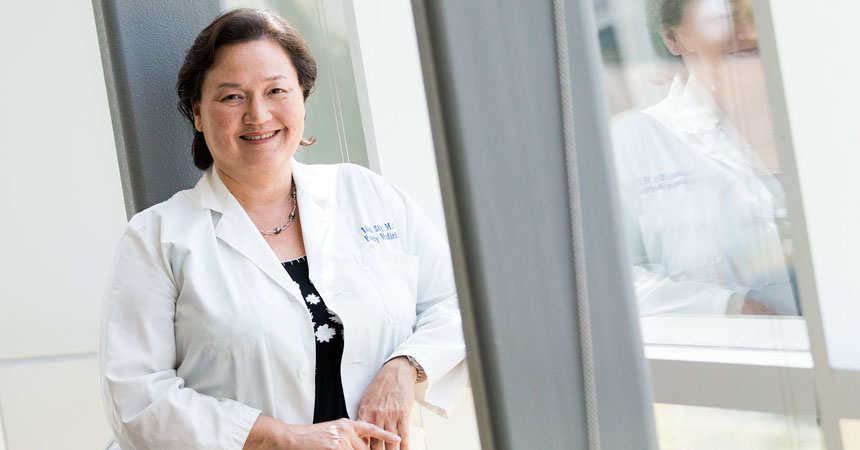
There was a time when Linda Siy, MD, was a Missouri girl through and through.
She was born and raised in Independence, Mo., famous as the home of President Harry Truman and the launching point for covered-wagon journeys westward on the Oregon Trail. She later earned a biology degree and a medical degree from the University of Missouri-Kansas City School of Medicine.
Meeting the physician shortageThe need Where young doctors spend their residencies often determines where they practice. Only 2 percent of the total residency slots in Texas are located in Fort Worth. The remedy A new agreement between UNTHSC, TCU and Medical City Healthcare will create 500 new residency slots in the Dallas-Fort Worth area in the next seven years. More such agreements are ahead. The result When their local residencies end, more doctors will stay in North Texas area to practice, helping alleviate the doctor shortage locally and statewide |
But when it was time for Dr. Siy to begin her promising medical career, she took her training and talents to Fort Worth, specifically to JPS Health Network’s family-medicine residency program. JPS hired her full-time in 1995. Dr. Siy, the past president of the Tarrant County Medical Society, has since cared for thousands of Texans.
Missouri’s loss was Texas’ gain.
“I was trained by the state of Missouri and its medical school. But I came to Texas for post-grad training, and I’ve stayed ever since,” said Dr. Siy, Assistant Professor at UNT Health Science Center. “When you enter into residency training, you develop connections to the community and ties to opportunities for jobs. It’s just natural that you’d stay.”
Dr. Siy’s journey to Fort Worth illustrates the transforming power of medical education – and why the partnership between UNTHSC and Texas Christian University is so critical to the future of health care in North Texas.
The new TCU and UNTHSC School of Medicine has gone from concept to reality in just four years, with an inaugural class of 60 students starting classes this month. Already, the school has served as a catalyst, bringing some of the region’s largest and most vital hospitals and health care systems to the table with a shared goal: to transform lives in North Texas through better health care.
The proof can be found in the creation of hundreds of new residency positions, ensuring that future Dr. Siys don’t have to leave home to establish their medical careers. The School of Medicine, working in partnership with UNTHSC’s original medical school, the Texas College of Osteopathic Medicine, will help make sure that more Texas-trained medical school graduates stay here.
The philosophy is simple, said Stuart Flynn, MD, founding Dean of the TCU and UNTHSC School of Medicine.
“Train them locally, keep them locally,” Dr. Flynn said.
Physician shortage
In 2016, Texas ranked 41st nationwide in physicians per capita and 47th in primary care doctors, according to the 2017 State Physician Workforce Data Report.
Texas, home to the most uninsured residents in the nation, also gained more new people last year than any other state, increasing its population to 29 million. The growth exacerbates the state’s physician shortage. Thirty-five Texas counties have no practicing physicians at all, while roughly 85 counties have fewer than five, according to Merritt Hawkins, a physician recruiting firm.
The shortage is not for lack of new medical schools. The TCU and UNTHSC School of Medicine will be the fourth new medical school to open in Texas since 2016, with two more coming online in the next few years.
“We’re getting to the point where we are training enough physicians,” Dr. Flynn said. “What we need is more GME.”
Graduate medical education, better known as residencies, is the three-year training period (minimum) that doctors undertake after graduating from medical school. During residencies, newly licensed physicians train under the guidance of experienced practitioners.
Nationwide, there are more medical school graduates than residency positions, meaning some new docs have nowhere to train. Their careers fizzle before they start. It’s a bad return on the huge investment that states make in training doctors.
Texas is on the right side of this equation for now, with more first-year residency positions (1,868) than estimated medical school graduates (1,722), according to the Texas Higher Education Coordinating Board. That is expected to change by 2021, unless someone can figure out a way to grow more residency positions.
“Texas invests in these medical students,” said W. Stephen Love, President and CEO of the Dallas-Fort Worth Hospital Council. “We need to do everything we can to keep them within the state of Texas.”
Enter UNTHSC, TCU and Medical City Healthcare. Last year, UNTHSC President Michael Williams, DO, MD, led efforts to create more local training opportunities for UNTHSC’s medical, pharmacy, physical therapy and physician assistant students, as well as develop new residency spots in Texas.
The result: Medical City has pledged to develop 500 new residency positions over the next seven years in its 14 hospitals across the Dallas-Fort Worth area. Other hospitals and health care systems are also planning residency partnerships with UNTHSC and TCU.
The new positions are key, especially in residency-starved Fort Worth, home to less than 2 percent of the state’s residency programs. Dallas, by comparison, has roughly 20 percent of Texas residency programs. Tarrant County has the capacity to create approximately 700 new residency positions, Dr. Flynn said.
The Texas Legislature has been doing its part to support graduate medical education as well. Prompted by Senator Jane Nelson of Flower Mound, state lawmakers increased biennium
funding for residencies from $14.3 million in 2014-2015 to $97.1 million in 2018-2019. In the most recent session, the Legislature approved a $60 million increase in graduate medical education grant funding to create more in-state residency slots.
Senator Nelson has praised the public-private partnership among UNTHSC, TCU and Medical City as essential to keeping more physicians in Texas.
“This partnership brings an established health care system with 14 hospitals in the Dallas-Fort Worth area together with a graduate university, without straining state resources,” she said. “It will be key in creating a pipeline of physician talent while ensuring our physicians are the best and brightest.”
Transforming medical education
UNTHSC spent years trying to establish an MD program. But the school didn’t find a feasible path forward until Dr. Williams invited TCU Chancellor Victor J. Boschini Jr. to breakfast in 2015 and pitched him on this innovative idea.
Dr. Williams, a UNTHSC alumnus, anesthesiologist and former hospital CEO, said it is past time for a new approach to medical school training, where educational models have remained largely static for decades. He wants medical students with exceptional communication skills, high levels of emotional intelligence and the ability to work in teams alongside pharmacists, PAs, PTs and other members of a health care team.
Most of all, he said, he wants UNTHSC-trained doctors to keep their patients at the center of everything they do.
“We’ve all seen how patients are treated in health care settings,” he said. “How can we get our physicians to focus on patients in a different way?”
At the new School of Medicine, students will follow patients very early in their training as part of their longitudinal integrated clerkships. In many medical schools, significant patient encounters don’t begin until the third year.
The curriculum will focus on communication, critical thinking, design and health care delivery systems. An Assistant Dean of Narrative Reflection and Patient Communication will help students build skills in awareness, listening, inquiry and engagement to foster better relations among physicians and their patients, their teams and their communities.
Med schools often are big drivers of research. UNTHSC, for example, received $52.4 million in research awards last year, much of it earned by faculty in the Graduate School of Biomedical Sciences. Dr. Flynn envisions more of the same for the School of Medicine, with an emphasis on partnering with Fort Worth biotechnology, pharmaceutical and life sciences firms.
“Medicine is changing as fast as you and I can breathe. Most places are training in a 2018 model, which is the 2008 model, which is the 1998 model,” Dr. Flynn said. “Where is medicine going to be 10 or 15 years from now? How are we preparing our students to be ready?
“Students want to come here. We want them to be here. And I want our curriculum to be so innovative that they’ll be saying, ‘I wonder what I get to learn today?’”







Social media