Medical Student Performance Evaluation

Professional Performance Statement
Professional standards are an integral part of the osteopathic profession and therefore a requirement for passing all preclinical and clinical courses through years 1-4. We expect all students to exhibit a high standard of professionalism at all times. This standard includes empathy, integrity, high moral ethics, motivation, and respect.
UNTHSC has adopted policies to govern student behavior that are designed to help them understand expectations and accept responsibility for their own actions. Information regarding the UNTHSC Student Code of Conduct can be found here.
Preclinical Coursework Description
All preclinical systems courses are graded on a Pass/Fail/Honors basis. Students move through a two pass sequence of organ system courses in the context of patient clinical presentations. The first pass emphasizes normal structure and function and basic principles of disease. The second pass integrates the previously learned material and expands it to focus on clinical presentations of common and important clinical conditions.
The Medical Practice courses apply and integrate the medical knowledge with the important psychomotor skills of physical examination, osteopathic manipulative medicine, communication, emotional intelligence, and other components involved in patient encounters.
The Professional Identity and Health Systems Practice Course is a mindful, purposeful course for students to develop their Professional Identity within the context of Health Systems Science. Students receive foundational content on: Ethics, Innovation, Patient Safety, Population/Public Health, Interprofessional Education, Health Promotion/Disease Prevention in years 1 and 2. Curriculum continues in year 3 as students apply their knowledge. Two examples of this application include:
1. Patient Safety. Students must successfully complete academic requirements and may sit for the Certified Professional in Patient Safety™ certification exam.
- The Texas College of Osteopathic Medicine (TCOM) in partnership with the Institute of Healthcare Improvement, is the only U.S. medical school offering the Patient Safety Course concluding with Patient Safety Certification opportunity awarded by the Certification Board for Professionals in Patient Safety.
- TCOM’s goal is to transform medical school curriculum to prepare future Certified Patient Safety Leaders in Medicine.
2. Innovation in medical education and healthcare is a necessity. Third year TCOM students choose a Health System problem they are passionate about, research and interview experts on ways others handle the problem and develop their own innovative solution called the iPOMP, Innovation Project on (my) Medical Passion to solve the issues. Students can use this project as a foundation for their Residency Performance Improvement Project.
Third Year Clerkships
Third Year Clerkships – MSPE Website
The objectives of the clinical clerkships are to equip TCOM students to achieve competence as graduates of an osteopathic medical school. The objectives and evaluation of the clerkship curriculum are represented by the AACOM Osteopathic Core Competencies for Medical Students.
- Osteopathic Principles
- Medical Knowledge
- Patient Care
- Professionalism
- Interpersonal & Communication Skills
- Practice-Based Learning & Improvement
- Systems-Based Practice
We introduce ACGME milestones during each core rotation specific to each specialty. Our end of the rotation evaluation incorporates feedback to students on many of the milestones in each specialty. This is to prepare the student to transition to residency with a solid understanding of level 1 or above in the milestone rubric.
Entrustable Professional Activities are measured and feedback is given to students during their core rotations in third year to prepare them to be first year residents upon completion of their trainingg at TCOM.
All core clinical clerkships are graded on an Honors/Pass/Fail basis. Students may be eligible for “Honors,” designated by the Clerkship Director, if they meet all expected requirements to pass the clerkship and:
- Score 91 or above on the COMAT exam for that clerkship (see below).
- Do not have a “Below Expectation” on any clinical evaluation competency
- Do not violate any Clinical Education policy or procedure while on the rotation, e.g. attendance
- The final designation for Honors is at the discretion of the Clerkship Director for Core clerkships and does not apply to elective rotations
The seven core clerkships with corresponding evaluation requirements are as follows:
Family Medicine
Final Honors/Pass/Fail determination based on successful completion of: Clinical Clerkship Evaluations, Internal Quizzes, COMAT Exam.
Internal Medicine
Final Honors/Pass/Fail determination based on successful completion of: Clinical Clerkship Evaluations, Online Learning Cases, Institute for Healthcare Improvement Patient Safety #103 and #104, COMAT Exam.
Obstetrics-Gynecology
Final Honors/Pass/Fail determination based on successful completion of: Clinical Clerkship Evaluations, Operative Reports, Weekly Quizzes, IHI Topic, COMAT Exam.
Osteopathic Manipulative Medicine
Final Honors/Pass/Fail determination based on successful completion of: Clinical Clerkship Evaluations, Pre-Rotation Quiz and Didactic Review Quiz, Institute for Healthcare Improvement Patient Safety #105, Weekly Clinic Log, COMAT Exam.
Osteopathic Manipulative Medicine is based on the ACGME specialty Osteopathic Neuromusculoskeletal Medicine and incorporates fundamentals of Neurology, PM&R, Sports Medicine, Orthopedic surgery, Radiology and Rheumatology.
Pediatrics
Final Honors/Pass/Fail determination based on successful completion of: Clinical Clerkship Evaluations, Weekly Aquifer Quizzes, IHI Topic, COMAT Exam.
Psychiatry
Final Honors/Pass/Fail determination based on successful completion of: Clinical Clerkship Evaluations, COMAT Exam.
Surgery
Final Honors/Pass/Fail determination based on successful completion of: Clinical Clerkship Evaluations, Weekly Projects, Weekly Discussion Postings, Draft Case Report, Final Case Report, COMAT Exam.
Additionally or students participate in Professional Identity and Health System practice courses including Patient safety. Patient safety is a two week required course in the third year that leads to the certification exam designating those who pass the exam as CPPS (Certified Professional in Patient Safety) by the Institute for Health Improvement.
COMAT Scores
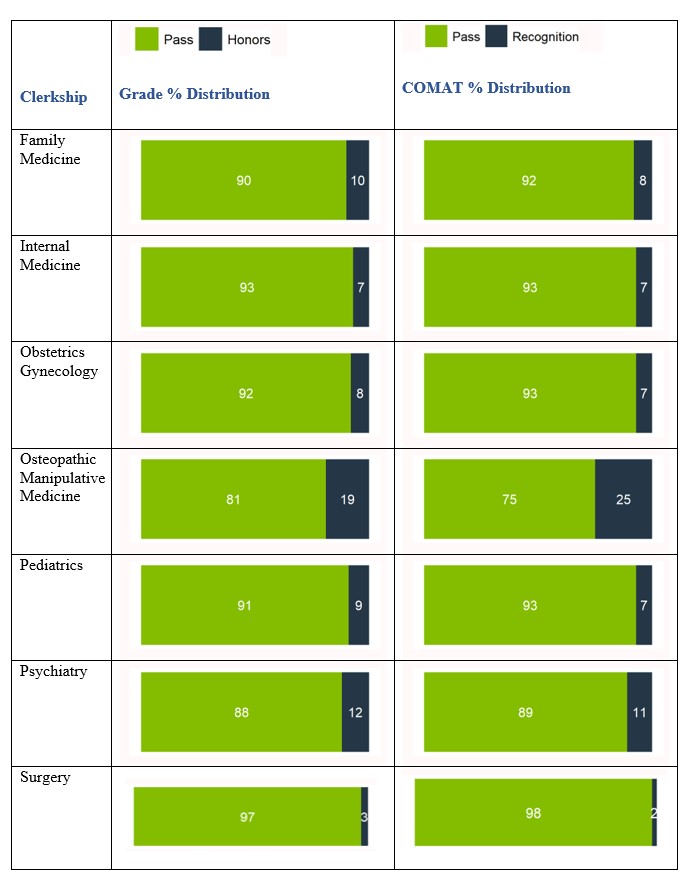
COMAT scores are reported by the NBOME as standardized scores based on national norms where the national mean is 100 and the standard deviation is 10. Typical scores fall within the range of 80 to 120. Since the COMAT score is used as part of the student’s clerkship grade, we scale the NBOME standardized score to a 100-point score. We employ a formula which sets the national mean (100) to a TCOM scaled score of 82, and anchors the score 1.7 standard deviations below the national mean (83) to a minimum passing score of 70. Scores are capped at 100. This formula is consistent across all COMAT subjects. Those who achieve an individual COMAT shelf exam score at or above the 90th percentile nationally receive Recognition for that exam.
Graphical class distribution indicating: 1) percentage of course Pass vs. Honors, and 2) percentage of COMAT Pass vs. Recognition (90th percentile or higher nationally)
COVID-19 Adjustments/Protocols
Clerkships
For the class of 2023, no disruptions or modifications due to COVID-19 occurred. However, the clinical education of the prior classes of 2021 and 2022 were disrupted due to COVID. For these previous cohorts, every student had a reduced in person clinical experience. The order of their rotations and their site assignments led to differing volumes of patient encounters in person and by telehealth. We assured their competencies through written and virtual evaluation of the learning objectives in the syllabi via alternative distant learning modules and meetings. COMAT exams were administered to assess medical knowledge.
During the COVID-19 pandemic, the National Board of Medical Examiners (NBOME) implemented a self-proctored version of the COMAT exam (COMAT-SP). During the 2020-2021 academic year, the COMAT-SP exam was administered remotely at the end of each core rotation, allowing students to take the exam safely in a remote setting. According to the NBOME, during the 2020-2021 testing cycle, 35 Colleges of Osteopathic Medicine administered the COMAT-SP (89% of all COMAT exams). None of these measures pertained to the TCOM class of 2023.
ROME/Rural Scholars
The ROME program at HSC is an innovative educational program designed to prepare students for life and practice in a rural and underserved community. Admission to the program will begin during the first semester of the first year. This rural medicine curriculum includes academic activities and clinical experiences that will continue throughout all four years of undergraduate medical education. Students accepted into the rural program, in addition to completing all regular curriculum courses during years 1 and 2, will have additional curriculum pertinent to rural and international medicine. These courses provide students with the opportunity to acquire the knowledge and skills needed for a career in rural medicine. The goals of the additional curriculum in the first two years are to help prepare the student for more hands-on patient care experiences and more independent learning in rural and international contexts.
In addition, Rural Scholar students have experiences with ROME faculty for early clinical encounters in an urban clinic that cares for underserved patients in Fort Worth. In Year 3, Rural Scholar students complete all of their core clinical rotations in rural communities to provide focused clinical training in a rural setting. During Year 3, students also complete a community health quality improvement project where they address a relevant health concern in their assigned community. Another notable experience includes the Agromedicine Workshop, which is an annual program hosted by the University of Texas-Tyler and the University of Iowa designed to provide training in the basics of diagnosis, treatment, and prevention of occupational and environmental injuries and illnesses within rural and agricultural communities.
ROME students also have opportunities to do elective rotations with ROME faculty in several international locations as well as mission trips to underserved communities in West Texas to further develop their skills and comfort in low resource settings.
Additional information about the Rural Scholars Program can be found at: https://www.unthsc.edu/texas-college-of-osteopathic-medicine/office-of-rural-medical-education/rome-rural-scholars-program/.
COMLEX Information
All students are required to have passed Level 1 and Level 2-CE of the Comprehensive Osteopathic Medical Licensing Examination (COMLEX-USA) before the DO degree will be awarded. COMLEX-USA is a three-level, national standardized examination series used by all medical licensing authorities to make licensing decisions for osteopathic physicians. It is designed to assess the osteopathic medical knowledge, knowledge fluency, and clinical skills considered essential for osteopathic generalist physicians to practice osteopathic medicine. COMLEX-USA examinations use a criterion-referenced standard-setting methodology. COMLEX-USA Level 1 is pass/fail, the minimum passing score for COMLEX-USA Level 2-CE is 400, with a mean score between 500 and 550. Passing Levels 1 and 2 means a candidate has demonstrated competence to enter into supervised clinical practice settings, enter graduate medical education, and prepare for lifelong learning.
Please see Overview of COMLEX-USA for additional details: https://www.unthsc.edu/career-center/wp-content/uploads/sites/71/COMLEX-Overview_revised.pdf
AACOM/NBOME joint press release: American Medical Association Officially Recognizes COMLEX- USA’s Equality with USMLE (December 4, 2018):
https://www.unthsc.edu/career-center/wp-content/uploads/sites/71/Press-Release_12-4-18_Formatted-for- MSPE.pdf
TCOM’s class of 2025 participated in the Clinical Competency Capstone (C3DO) pilot assessment in partnership with the National Board of Osteopathic Medical Examiners (NBOME). This eight-station OSCE assesses osteopathic medical student performance in the skills of patient interviewing, physical exam, osteopathic manipulation, humanism, and clinical reasoning. All students are required to achieve appropriate competence in these areas to graduate.
TOUCH
Translating Osteopathic Understanding into Community Health (TOUCH) is a national initiative of the Council of Osteopathic Student Government Presidents (COSGP). This program encourages osteopathic medical students to engage in service throughout their community in order to impact those outside of osteopathic medical students and professionals. The purpose of the program is to expand osteopathic ideals and principles to those unaware of our profession’s values. In accordance with the osteopathic philosophy of treating the whole patient, service goes beyond mere health promotion and can include a wide array of involvement that has a strong positive impact on people’s lives. Learn more about the program here.
Medical School Information
Discover TCOM – Texas College of Osteopathic Medicine (unthsc.edu)


Social media